KNOXVILLE, TN, January 16, 2026 /24-7PressRelease/ -- Accurate, continuous blood pressure (BP) monitoring is essential for preventing cardiovascular events, yet conventional cuffs and wearable sensors often suffer from discomfort, motion interference, and poor alignment. This study demonstrates a minimally invasive, subcutaneously implanted ultrasonic device capable of capturing real-time arterial diameter changes to derive precise BP values.
Hypertension remains one of the world's leading causes of heart disease, stroke, and premature mortality. Although regular blood pressure tracking can significantly reduce cardiovascular risks, traditional cuff-based measurements disrupt daily activity and are unsuitable for continuous monitoring. Alternatives such as photoplethysmography (PPG) and wearable ultrasound patches attempt to address these limitations but often struggle with shallow penetration depth, dependence on gels, and significant sensitivity to misalignment or motion. Implantable sensors have emerged as a potential solution, yet many require intrusive placement inside arteries or suffer from foreign-body reactions at the interface. Due to these challenges, there is a need for deeper research on reliable, non-intrusive implantable systems for continuous blood pressure (BP) assessment.
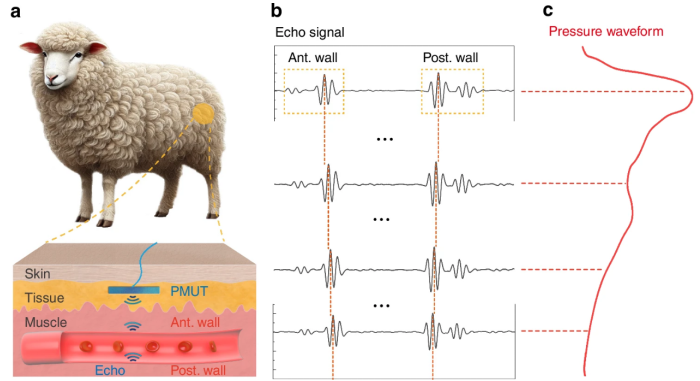
Researchers from the University of California, Berkeley, and collaborating institutions report a new implantable ultrasound-based blood pressure monitoring system in a paper published (DOI: 10.1038/s41378-025-01019-w) in Microsystems & Nanoengineering on November 6, 2025. The study presents a subcutaneous device built on a 5 × 5 mm² piezoelectric micromachined ultrasonic transducers (PMUTs) array that continuously measures arterial diameter changes to reconstruct BP waveforms. Through comprehensive laboratory validation and an in vivo implantation in an ambulatory sheep, the team demonstrates that the device achieves clinically reliable systolic and diastolic measurements with minimal calibration error.
The newly developed system relies on a dense 37 × 45 PMUT array fabricated using CMOS-compatible processes. Each PMUT features a 29-µm diaphragm and operates at approximately 6.5 MHz in water, enabling high axial resolution and strong echo penetration through tissue. The dual-electrode bimorph design significantly enhances acoustic output, while an optimized deep reactive ion etching (DRIE) process ensures high structural uniformity across the array.
To derive blood pressure, the device measures the time-of-flight between ultrasound echoes reflected from the anterior and posterior arterial walls. This time interval is converted into a real-time diameter waveform, which correlates directly with blood pressure through vessel stiffness models. Bench-top tube experiments confirmed the linear relationship between diameter and pressure, and simulations revealed that wearable systems can lose up to 60% signal strength with only 1 mm of misalignment—an issue the implanted design avoids.
During in vivo testing, researchers implanted the PMUT system above the femoral artery of an adult sheep. The device successfully captured detailed pressure waveforms, including features such as the dicrotic notch, and matched gold-standard arterial line measurements within −1.2 ± 2.1 mmHg (systolic) and −2.9 ± 1.4 mmHg (diastolic). These results demonstrate that the minimally invasive design maintains stable coupling and accurate long-term performance.
"The study shows that ultrasound-based implants can achieve the stability and precision required for continuous blood pressure monitoring without the drawbacks of cuffs or fragile wearables," said the corresponding author. "By capturing arterial diameter changes directly through subcutaneous sensing, the device avoids issues like gel dependence, environmental noise, and misalignment. Our findings suggest that this technology could support long-term hypertension management and provide clinicians with richer cardiovascular data than periodic measurements allow."
This implantable PMUT-based system represents a promising alternative to conventional BP monitoring tools for patients requiring continuous, unobtrusive measurement. Its stability against tissue growth, motion, and environmental interference makes it particularly suitable for long-term hypertension management, early detection of cardiovascular abnormalities, and integration into digital health platforms. Future advances—such as beamforming to mitigate positional shifts and data-driven analytics for individualized risk prediction—could further expand its clinical utility. Ultimately, this technology may enable preventive care strategies by providing continuous, high-fidelity cardiovascular data in real-world environments.
References
DOI
10.1038/s41378-025-01019-w
Original Source URL
https://doi.org/10.1038/s41378-025-01019-w
Funding Information
This work was supported in part by BSAC (Berkeley Sensor and Actuator Center).
About Journal
Microsystems & Nanoengineering
Chuanlink Innovations, where revolutionary ideas meet their true potential. Our name, rooted in the essence of transmission and connection, reflects our commitment to fostering innovation and facilitating the journey of ideas from inception to realization.
Related Link:
http://chuanlink-innovations.com
# # #
Contact Information
George Hua
Chuanlink Innovations
Knoxville, Tennessee
USA
Telephone: 8656606278
Email: Email Us Here
Website: Visit Our Website